Call Us For Easy
Confidential Assistance
503-506-0101
It only takes 5 minutes to get started
The Dangers of ‘Cold Turkey’ Detox: Why Medical Supervision is Critical
Posted on: January 1st, 2026 by writer

Table of Contents
- The Neuroscience of Withdrawal: Why Your Brain Can’t Hit the Brakes
- The Timeline of Danger: How Withdrawal Escalates from Uncomfortable to Fatal
- The “Kindling Effect”—Why Past Success Means Nothing
- Why Benzodiazepines Are Even More Dangerous to Quit Cold Turkey
- The Hidden Cost of Cold Turkey: Why Unassisted Detox Sets You Up for Relapse
- The Choice That Could Save Your Life: Home Detox vs. Professional Medical Supervision
- The Pacific Northwest Context: Why Oregon Needs More Medical Detox Access
- Final Thoughts
The phrase “going cold turkey” sounds bold—even admirable. For many, quitting alcohol or benzodiazepines abruptly feels like the ultimate test of willpower. But what most people don’t realize is that for certain substances, cold turkey detox isn’t brave—it’s biologically dangerous. Unlike quitting caffeine or nicotine, stopping alcohol or benzodiazepines suddenly can trigger life-threatening medical emergencies, including seizures, cardiac arrest, and a condition called Delirium Tremens (DTs), which historically killed more than one-third of those who experienced it. Even today, untreated severe withdrawal carries mortality rates between 1% and 5%.
At Pacific Ridge in Jefferson, Oregon, we provide medically supervised detox because we understand what happens inside your body when you stop drinking. This article explains the neuroscience of why cold turkey detox is so dangerous—and why professional supervision isn’t just safer, it’s lifesaving.
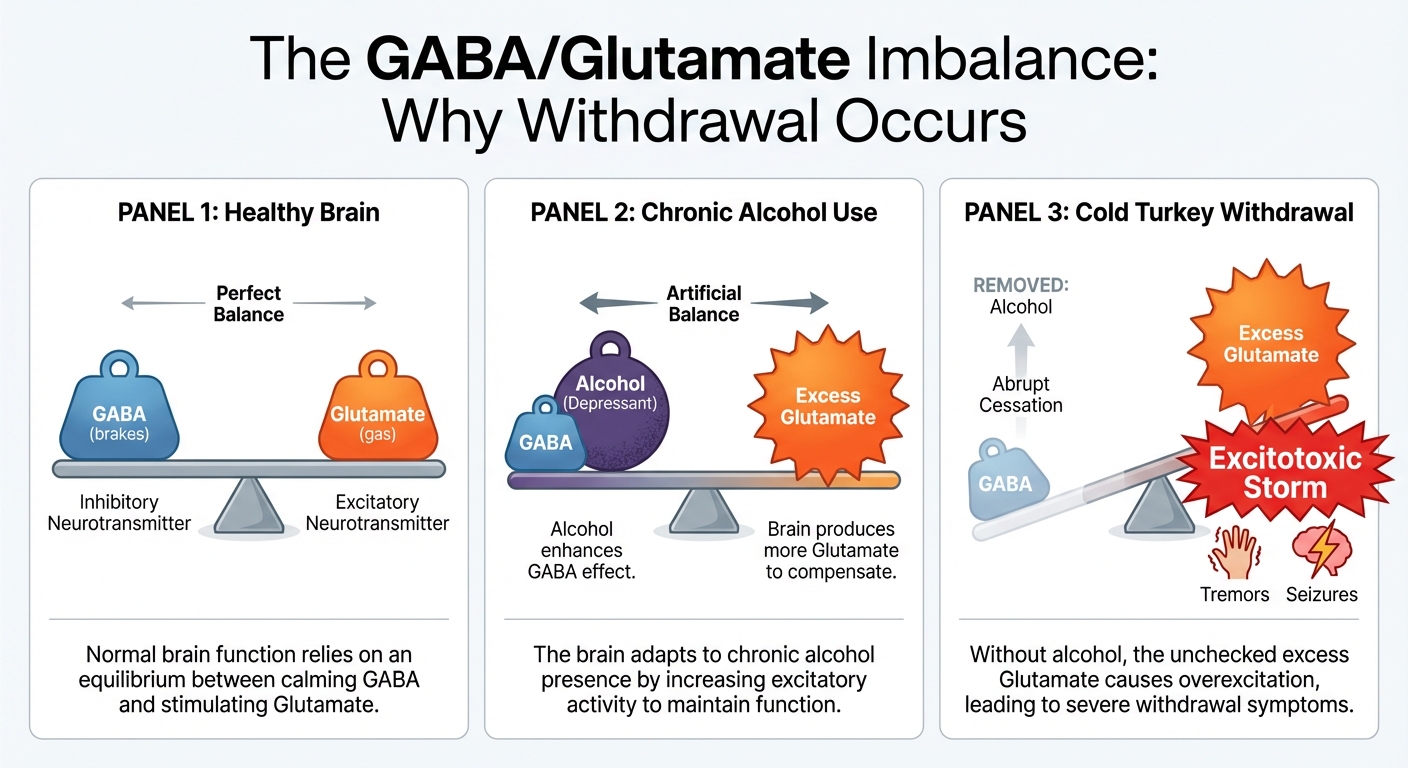
The Neuroscience of Withdrawal: Why Your Brain Can’t Hit the Brakes
To understand why cold turkey detox is dangerous, you need to understand how alcohol rewires your brain chemistry—and what happens when you suddenly remove it. Alcohol is a central nervous system (CNS) depressant that works by enhancing GABA (the brain’s “calm down” neurotransmitter) and suppressing Glutamate (the brain’s “speed up” neurotransmitter). Think of GABA as the brake pedal in your brain, while Glutamate acts as the accelerator. When alcohol is present, it’s like constantly pressing down on the brake. Over months and years of heavy drinking, your brain compensates by making two critical adjustments:
- Downregulating GABA receptors (making them less sensitive, so you need more alcohol to feel the same calming effect)
- Upregulating Glutamate receptors (creating more of them to counteract alcohol’s depressive effects)
When you stop drinking abruptly, the sedative “brakes” (GABA) are suddenly gone, but the excitatory “accelerator” (Glutamate) is stuck on full power. The result? A state of excitotoxic hyperactivity—your neurons fire uncontrollably, leading to tremors, elevated heart rate, dangerously high blood pressure, and in severe cases, seizures and brain damage.
The Metabolic Storm You Can’t See
Beyond neurotransmitters, withdrawal causes severe electrolyte imbalances that dramatically increase your risk of fatal cardiac events:
- Hypomagnesemia (low magnesium) and Hypokalemia (low potassium) are common in alcohol withdrawal and directly increase the risk of fatal cardiac arrhythmias
- Severe vomiting and sweating during unassisted detox worsen these imbalances, creating a dangerous feedback loop
- Your heart’s electrical system depends on precise electrolyte levels—when they’re off, your heart can stop
The bottom line: Withdrawal isn’t a psychological challenge—it’s a physiological emergency. Your brain’s chemistry is in chaos, and willpower cannot regulate neurotransmitters.
The Timeline of Danger: How Withdrawal Escalates from Uncomfortable to Fatal
Alcohol withdrawal follows a predictable progression. Understanding this timeline reveals why the first 48-96 hours are the most dangerous—and why medical monitoring is critical.
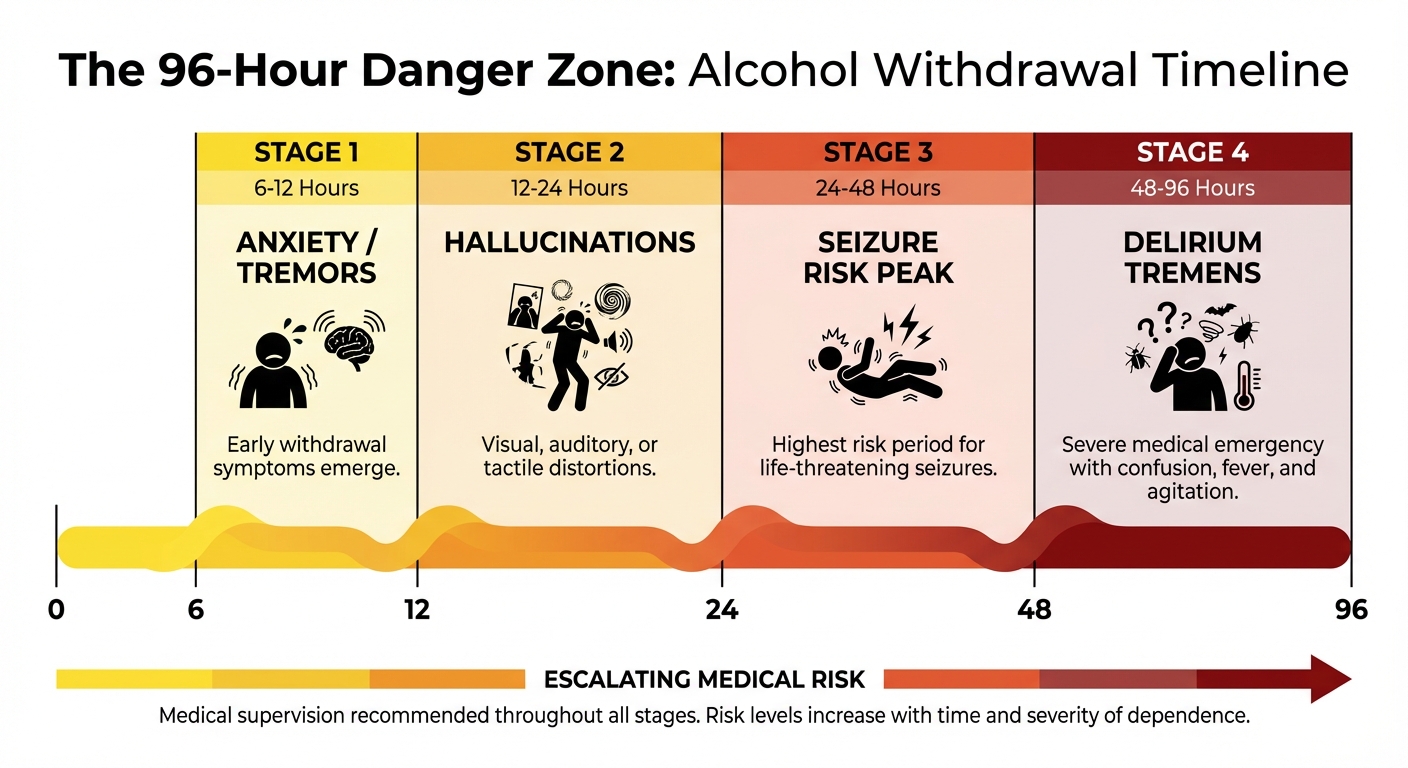
Stage 1: Minor Withdrawal (6-12 Hours)
Within hours of your last drink, your body begins to react. You might experience anxiety, insomnia, nausea, mild tremors, and heart palpitations. While these symptoms are uncomfortable, they’re setting the stage for what could come next. This is when your brain’s chemistry starts shifting dangerously.
Stage 2: Moderate Withdrawal (12-24 Hours)
As your brain’s excitatory system gains momentum, visual or auditory hallucinations may begin. Your tremors become more severe. This is the critical window where medical intervention with benzodiazepine tapering can prevent the next, potentially fatal stage. Many people underestimate the danger at this point because they’re “managing” the symptoms—but your seizure risk is climbing rapidly.
Stage 3: Severe Withdrawal (24-48 Hours)
This is when withdrawal becomes life-threatening. Generalized tonic-clonic seizures can occur without warning. During a seizure, you can aspirate (inhale vomit into your lungs), suffer head trauma from falling, or experience cardiac arrest. Even if the seizure itself doesn’t kill you, the complications can. This stage requires immediate medical intervention with anticonvulsant therapy.
Stage 4: Critical Withdrawal (48-96 Hours) – Delirium Tremens
Delirium Tremens (DTs) represents the most severe form of alcohol withdrawal, occurring in 3-5% of people who experience withdrawal. For those who develop DTs outside a medical setting, the condition remains almost universally fatal. Symptoms include:
- Global confusion and disorientation (not knowing where you are, who you are, or what’s happening)
- Severe agitation and terrifying hallucinations
- Profuse sweating and dangerously high body temperature (hyperthermia)
- Extreme tachycardia (rapid heartbeat) and hypertension
- High risk of aspiration pneumonia (inhaling vomit into lungs)
Before modern intensive care, DTs killed 37% of patients. Even today, mortality remains between 1-5% with medical treatment—but untreated DTs are almost universally fatal due to cardiovascular collapse, hyperthermia, or aspiration.
The Case That Illustrates the Stakes
A 45-year-old man with a 10-year drinking history attempted home detox. At 36 hours, he suffered a grand mal seizure while alone, resulting in head trauma and aspiration pneumonia. He required ICU admission and intubation. His story illustrates a critical truth: withdrawal severity is biological, not a reflection of character or willpower.
The “Kindling Effect”—Why Past Success Means Nothing
Many people believe that because they’ve detoxed at home before, they can do it again. This is dangerously wrong. The Kindling Effect describes how repeated withdrawal episodes progressively lower your seizure threshold. It’s like a forest fire that’s been put out but leaves the ground more flammable for the next fire. Each time you go through withdrawal and then relapse, you’re not starting from zero—you’re starting from a more vulnerable position. Here’s what this means in practice:
- Each time you withdraw and relapse, the next withdrawal becomes more severe and dangerous—even if you drank less
- Someone who had mild tremors during their first detox may experience a full seizure during their second attempt
- The protective mechanisms in your brain become progressively damaged with each withdrawal cycle
- Your risk compounds exponentially, not linearly
Past survival of cold turkey detox does not predict future safety—it predicts increased future risk. Every time you roll the dice, the odds get worse.
Why Benzodiazepines Are Even More Dangerous to Quit Cold Turkey
If you’ve been taking benzodiazepines (Xanax, Valium, Klonopin) alongside alcohol—or on their own—the risks of sudden cessation are equally severe and often more prolonged. Benzodiazepines work on the same GABA receptors as alcohol, meaning withdrawal follows the same dangerous neurochemical pathway. However, there are critical differences that make benzodiazepine withdrawal particularly treacherous:
Equal or Greater Seizure Risk
Sudden benzodiazepine cessation carries an equal or higher seizure risk compared to alcohol withdrawal. The FDA now requires a black box warning on benzodiazepines specifically highlighting the dangers of sudden cessation and the need for medically supervised tapering.
Protracted Withdrawal Syndrome
Unlike alcohol, where acute detox typically resolves in 5-7 days, benzodiazepine withdrawal can cause ongoing symptoms for weeks or even months. This includes:
- Persistent anxiety and panic attacks
- Insomnia and sleep disturbances
- Cognitive fog and difficulty concentrating
- Physical tension and muscle pain
These prolonged symptoms make unsupervised withdrawal not just dangerous in the acute phase, but nearly impossible to maintain long-term without professional support.
The Deadly Combination
Many individuals use alcohol and benzodiazepines together, creating a synergistic toxicity during withdrawal. A 32-year-old woman stopped both substances abruptly and developed severe psychosis, tachycardia, and required intubation and high-dose sedation to stabilize. Mixed withdrawal creates compounded risks that are nearly impossible to manage safely at home.
Why Medical Tapering Is Non-Negotiable
Benzodiazepine detox requires a slow, controlled taper over weeks or months to allow GABA receptors to gradually normalize. Abrupt cessation doesn’t give the brain time to recalibrate, leading to severe rebound anxiety, seizures, and psychological distress.
The Hidden Cost of Cold Turkey: Why Unassisted Detox Sets You Up for Relapse
Even if someone survives the acute dangers of cold turkey detox, they often face weeks or months of Post-Acute Withdrawal Syndrome (PAWS)—a lesser-known but powerful driver of relapse.
What Is PAWS?
PAWS is a cluster of ongoing symptoms that persist after acute withdrawal has ended. While your body may have cleared the alcohol or benzodiazepines, your brain is still healing from the neurochemical damage. During this time, you may experience:
- Cognitive fog and difficulty concentrating (feeling like you’re thinking through mud)
- Emotional numbness or extreme irritability
- Sleep disturbances that can last for months
- Intense, unpredictable cravings that seem to come out of nowhere
PAWS can last weeks to months, and during this time, the brain is still healing from years of substance-induced changes.
The Relapse Trap
Here’s the cruel irony: People who detox cold turkey often relapse not because they lack willpower, but because PAWS symptoms become unbearable without medical and therapeutic support. When your brain is constantly sending distress signals—when you can’t sleep, can’t think clearly, and experience waves of emotional chaos—the temptation to “feel normal again” by drinking becomes overwhelming.
How Medical Detox Reduces PAWS
Medical detox doesn’t just get you through the acute danger zone—it sets you up for long-term success:
- Pharmacological smoothing: Medications used during medical detox (benzodiazepine tapers, anti-seizure medications, vitamins) help ease the neurochemical transition, potentially reducing PAWS severity
- Nutritional intervention: IV fluids, thiamine (Vitamin B1), and electrolyte replacement prevent Wernicke-Korsakoff Syndrome, a form of alcohol-related brain damage that worsens cognitive symptoms
- Structured transition: Medical detox bridges patients into residential rehab with a clearer mind and stabilized body, setting the foundation for psychological recovery work
The Two Paths
Cold turkey detox often ends in one of two ways:
- Medical emergency (seizure, DTs, cardiac event)
- Rapid relapse due to unbearable PAWS symptoms and lack of support structure
Medical detox addresses both risks simultaneously, protecting your brain during the vulnerable healing phase and giving you a real chance at long-term recovery instead of a cycle of relapse.
The Choice That Could Save Your Life: Home Detox vs. Professional Medical Supervision
This comparison provides a clear, evidence-based look at why medical detox is not a luxury—it’s a medical necessity.
| Category | Home Detox | Medical Detox at Pacific Ridge |
|---|---|---|
| Safety | High risk of seizures, aspiration, cardiac arrest, and Delirium Tremens. No medical intervention available when complications arise. | 24/7 vital sign monitoring with immediate medical intervention for complications. Trained staff can respond within seconds to any emergency. |
| Comfort & Symptom Management | Extreme physical distress including vomiting, hallucinations, severe tremors, and insomnia with no relief available. | Pharmacological support including benzodiazepine taper protocols and anti-nausea medications to significantly reduce suffering while maintaining safety. |
| Seizure Prevention | No medical intervention. Seizures can cause brain damage, aspiration, head trauma, or death. | Prophylactic anti-seizure protocols with staff trained to respond immediately. Medical supervision reduces seizure occurrence by up to 90%. |
| Nutritional & Metabolic Support | Likely severe dehydration, vitamin deficiency (especially thiamine), and electrolyte imbalances that increase cardiac risk. | IV fluids, thiamine infusions, and electrolyte replacement to prevent Wernicke-Korsakoff Syndrome and cardiac complications. |
| Success Rate & Completion | Very low. Unbearable symptoms typically lead to immediate relapse to stop the pain. | High. Patients stabilize and transition to residential therapy with clear cognition and a foundation for recovery. |
| Neurological Protection | Risk of permanent excitotoxic brain damage from uncontrolled Glutamate storms. | Neuroprotective medications minimize brain stress and long-term cognitive impact. |
| Psychological Support | Isolation, fear, confusion, and no framework for understanding what’s happening to your body. | Compassionate clinical team providing support and education. Preparation for therapeutic work begins during detox, not after. |
The Statistical Imperative
Untreated Delirium Tremens carries a mortality rate between 1-5% even with late medical intervention; historically, mortality was 37% before modern protocols. Medical detox reduces seizure occurrence by up to 90% through controlled benzodiazepine tapering and continuous monitoring.
Why “Toughing It Out” Isn’t Strength—It’s Risk
Many people believe that enduring cold turkey detox demonstrates commitment or strength. In reality:
- Withdrawal severity is entirely biological, determined by receptor downregulation, electrolyte balance, and genetic factors—not character
- Choosing medical supervision demonstrates informed self-care and a commitment to survival, not weakness
- The bravest choice is the one that gives you the best chance of living to complete your recovery journey
Pacific Ridge’s Approach
At Pacific Ridge, medical detox combines:
- Round-the-clock nursing and physician oversight
- Evidence-based medication protocols tailored to individual withdrawal severity
- A serene, private environment on 18 acres in Jefferson, Oregon—medical safety without the institutional feel
- Seamless transition into residential therapy once stabilization is achieved
The choice isn’t between “easy” and “hard”—it’s between dangerous and safe. Medical detox removes the life-threatening variables so you can focus on the real work: long-term recovery.
The Pacific Northwest Context: Why Oregon Needs More Medical Detox Access
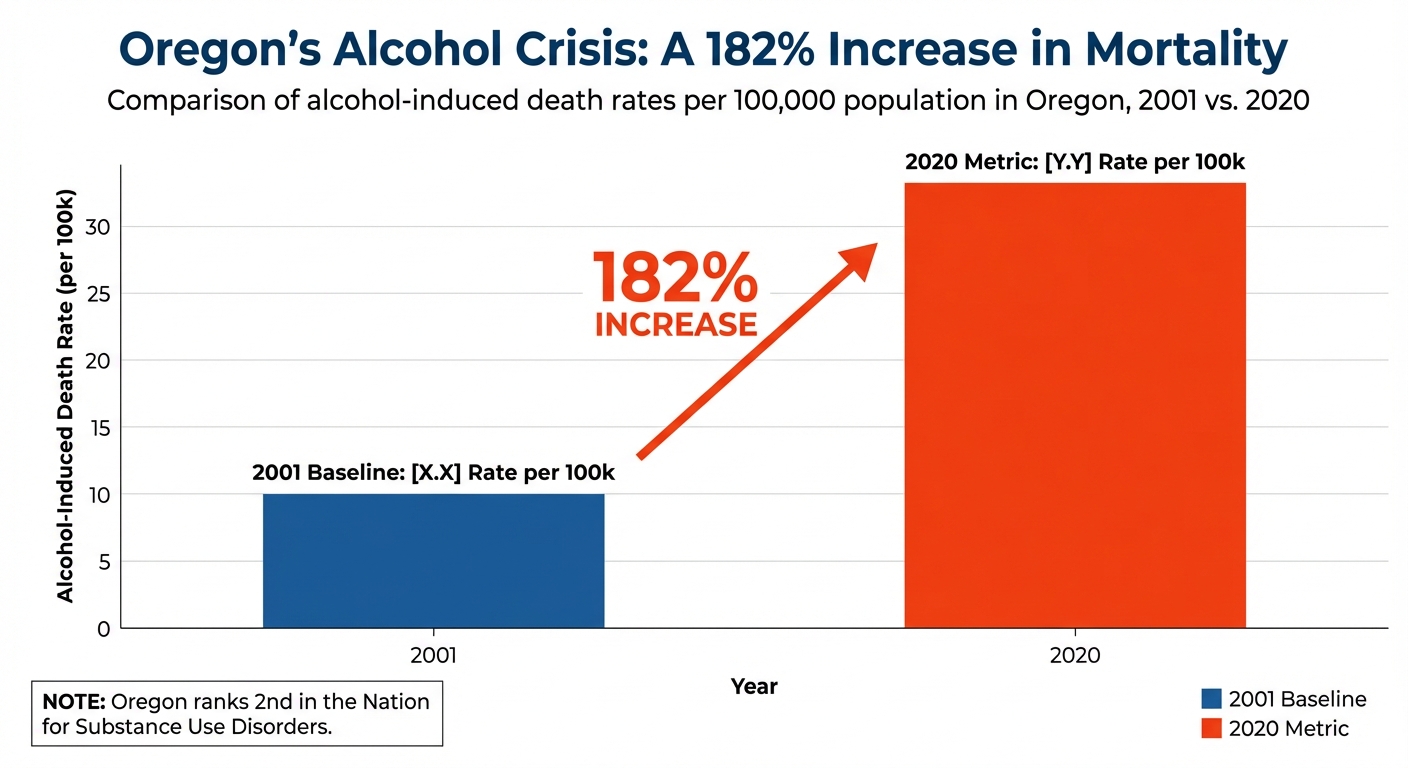
Oregon faces unique and severe challenges regarding substance use disorders, making facilities like Pacific Ridge not just helpful—but critical infrastructure.
The Numbers Tell a Stark Story
- National Ranking: Oregon ranks 2nd in the nation for adult substance use disorder rates according to the 2021 National Survey on Drug Use and Health
- Alcohol Mortality Surge: Between 2001 and 2020, alcohol-induced death rates in Oregon increased by 182%
- Treatment Gap: Despite high need, Oregon ranks near the bottom nationally for access to treatment services, creating dangerous delays for individuals in crisis
What This Means for You and Your Community
Oregon’s emergency rooms are overwhelmed with withdrawal-related crises that could have been prevented with early access to medical detox. Private, specialized facilities like Pacific Ridge alleviate pressure on hospital systems while providing higher-quality, individualized care. Geographic accessibility matters: Pacific Ridge’s location in Jefferson serves the Salem, Portland, and Eugene corridors, offering a regional solution to a statewide problem.
The Community Ripple Effect
When individuals attempt cold turkey detox at home:
- Families often call 911 during seizures or DTs, burdening emergency services and first responders
- Survivors may suffer permanent brain damage from seizures or Wernicke-Korsakoff Syndrome, creating long-term healthcare costs and family caregiver burden
- High relapse rates perpetuate cycles of crisis and hospitalization, straining both families and the healthcare system
The Pacific Ridge Solution
Professional medical detox:
- Prevents emergencies rather than reacting to them after the damage is done
- Provides a direct pathway from crisis stabilization to residential therapy, increasing long-term recovery success
- Offers a private, compassionate alternative to institutional emergency settings
Oregon’s addiction crisis requires scalable, accessible medical detox services. Choosing professional care doesn’t just protect individuals—it strengthens entire communities by breaking the cycle of crisis and creating pathways to lasting recovery.
Final Thoughts
The term “cold turkey” may sound like a test of willpower, but the medical reality is far more dangerous. When you stop drinking alcohol or taking benzodiazepines abruptly, your brain enters a state of neurochemical chaos—GABA depletion, Glutamate storms, electrolyte collapse, and seizure risk. For 3-5% of people, this escalates to Delirium Tremens, a condition that remains life-threatening even with modern medicine. The evidence is clear: Cold turkey detox isn’t brave—it’s biologically reckless. Medical supervision transforms a potentially fatal process into a managed, safe transition. At Pacific Ridge in Jefferson, Oregon, we provide 24/7 medical oversight, evidence-based medication protocols, and compassionate care in a private, serene environment. Our approach isn’t just about getting you through detox—it’s about protecting your brain, stabilizing your body, and setting the foundation for lasting recovery. If you or someone you love is considering detox, the choice isn’t between easy and hard—it’s between dangerous and safe. Medical detox saves lives. It’s that simple.
Ready to Take the First Step Toward Safe Recovery?
If you’re ready to take the first step toward safe, medically supervised detox, contact Pacific Ridge today. Your brain—and your future—deserve professional care.
References:
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). (2022). Neuroscience: Pathways to Alcohol Dependence. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/neuroscience-pathways-alcohol-dependence
- National Library of Medicine. (2022). Electrolyte Disturbances in Alcohol Withdrawal. https://pubmed.ncbi.nlm.nih.gov/2406606/
- National Library of Medicine (StatPearls). (2023). Delirium Tremens. https://www.ncbi.nlm.nih.gov/books/NBK482134/
- New England Journal of Medicine. (2014). Recognition and Management of Withdrawal Delirium (Delirium Tremens). https://www.nejm.org/doi/full/10.1056/NEJMra1407298
- Alcohol Health & Research World. (1998). Kindling in Alcohol Withdrawal. https://pubs.niaaa.nih.gov/publications/arh22-1/25-34.pdf
- Food and Drug Administration (FDA). (2020). FDA Drug Safety Communication: FDA requiring Boxed Warning updated to improve safe use of benzodiazepine drug class. https://www.fda.gov/drugs/drug-safety-and-availability/fda-requiring-boxed-warning-updated-improve-safe-use-benzodiazepine-drug-class
- UCLA Health. (2023). Post-Acute Withdrawal Syndrome (PAWS). https://www.semel.ucla.edu/dual-diagnosis-program/conditions/post-acute-withdrawal-syndrome
- SAMHSA. (2021). 2021 National Survey on Drug Use and Health (NSDUH) Releases. https://www.samhsa.gov/data/release/2021-national-survey-drug-use-and-health-nsduh-releases
- Oregon Health Authority. (2022). Alcohol-Induced Death Rates in Oregon. https://www.oregon.gov/oha/PH/PREVENTIONWELLNESS/SUBSTANCEUSE/ALCOHOL/Pages/index.aspx
- National Center for Biotechnology Information (NCBI). (2015). Complications of Alcohol Withdrawal. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6761825/
- SAMHSA. (2021). Detoxification and Substance Abuse Treatment: A Treatment Improvement Protocol (TIP 45). https://store.samhsa.gov/product/TIP-45-Detoxification-and-Substance-Abuse-Treatment/SMA15-4131
Posted in Treatment
Recent Posts
- From Pills to Fentanyl: Understanding the Progression of Opioid Addiction
- Sober Activities in the Willamette Valley: Rediscovering Life Without Substances
- Cannabis Hyperemesis Syndrome (CHS): The Physical Reality of Chronic Marijuana Use
- Protecting Your Career While Seeking Treatment: FMLA and Privacy Rights for Oregon Employees
Are you looking for help?
Pacific Ridge is a residential drug and alcohol treatment facility about an hour from Portland, Oregon, on the outskirts of Salem. We’re here to help individuals and families begin the road to recovery from addiction. Our clients receive quality care without paying the high price of a hospital. Most of our clients come from Oregon and Washington, with many coming from other states as well.
Pacific Ridge is a private alcohol and drug rehab. To be a part of our treatment program, the client must voluntarily agree to cooperate with treatment. Most intakes can be scheduled within 24-48 hours.
Pacific Ridge is a State-licensed detox and residential treatment program for both alcohol and drugs. We provide individualized treatment options, work closely with managed care organizations, and maintain contracts with most insurance companies.
Quick links
Recent Posts
- From Pills to Fentanyl: Understanding the Progression of Opioid Addiction
- Sober Activities in the Willamette Valley: Rediscovering Life Without Substances
- Cannabis Hyperemesis Syndrome (CHS): The Physical Reality of Chronic Marijuana Use
- Meth-Induced Psychosis: Understanding the Brain’s Recovery Timeline
Contact Us
Pacific Ridge- 1587 Pacific Ridge Ln SE
Jefferson, OR 97352 - Email:
[email protected] - Phone:
503-506-0101 - Fax:
503-581-8292
- Copyright © 2026 Pacific Ridge - All Rights Reserved. Web Design & SEO by Lithium
- Follow us on

